Conditions Treated by End Vas Int
Peripheral Arterial Disease (PAD)
Peripheral arterial disease (PAD) is a common condition affecting 1 in 20 persons age 50 and older. PAD happens when arteries in the legs narrow, reducing or cutting off blood flow, and is a leading cause of non-trauma related amputations when not diagnosed and treated early. More than 400 non-traumatic amputations happen every day as a result of PAD.
Symptoms & Signs
Could it be PAD? What are the signs and symptoms of peripheral arterial disease?
Signs and symptoms of PAD can easily go unrecognized or be dismissed. Leg pain that occurs while walking and stops with rest is one of the first symptoms of PAD, but 91% of Americans (local data not available) would dismiss leg pain as just part of getting older. You may have PAD if you experience the following:
- One foot may feel colder than the other.
- Your foot or leg may become pale, discolored or blue.
- Leg weakness or numbness may make you feel off-balance or make it harder to walk.
- Your toenails and leg hair may stop growing.
- You may have pain or a feeling of pins and needles in your leg or foot.
- Sores or wounds on your toes, feet or legs may appear, heal slowly or not heal at all.
Lifestyle changes and medical management
Early stages of PAD can often be treated with lifestyle changes. Exercise, a heart-healthy diet and quitting tobacco use can alleviate symptoms and prevent further progression of the disease.
In addition, medications that lower cholesterol or control high blood pressure may be prescribed. Other medications that prevent blood clots or the buildup of plaque in the arteries may also be prescribed. Management with medication has been shown to significantly increase pain-free walking distance and total walking distance in individuals with intermittent claudication.
An interventional radiologist can prescribe such treatments and monitor your condition through regular follow-up visits to monitor disease progression. An IR will also work with your care team.
Interventional Option:
If you have later-stage PAD, or if lifestyle changes and medical management aren’t enough to treat your PAD, you might benefit from a minimally invasive interventional radiology treatment. These treatments for those with severe symptoms not relieved by lifestyle changes alone help to remove blockages and preserve toes and limbs.
In most cases, the End VIR will make a small incision in your groin and, using X-rays or Flouroscope imaging to guide him, thread a very thin catheter through your blood vessels to the blockage or narrowed artery. Depending on where the blockage is and how it looks, it may be treated in several ways.
Angioplasty:
Angioplasty uses inflatable devices called balloons to open up narrowed arteries. Various types of balloons are used in different situations, including balloons that stretch arteries open, metal-edged balloons that cut and break up calcium deposits, and drug-coated balloons that can prevent scarring and future narrowing of the artery. During angioplasty, the Endovascula interventionist guides a catheter with a tiny balloon tip through the blood vessels into the blockage. The balloon is inflated to widen the artery, which restores blood flow.
Stenting:
Sometimes, following balloon angioplasty, the doctor will place a stent (a tiny mesh tube) in the artery to help keep it open. Those who receive stents will also need to be on clot-preventing medications to reduce the chance of clots forming inside the stent.
Thrombolysis:
Thrombolysis, which is usually enacted in an emergency because the body has not had enough time to respond by growing new blood vessels to bypass the blockage, is a treatment that delivers medication slowly, over 12–24 hours, to a blood clot through a thin tube that is inserted next to or within the clot. You’ll be hospitalized during the treatment and will be watched by nurses and doctors in the intensive care unit. Often, the clots will dissolve but the artery will still be narrowed, and additional treatments may be required.
Thrombectomy: When a blood clot suddenly blocks blood flow, a treatment known as a thrombectomy will remove the clot from the body using various medical tools that can draw out, pull out, or vaporize the clot.
What can I expect after treatment?
Once the treatment is completed, the End Vas Int removes the catheter and applies pressure to the tiny incision in your groin to allow it to heal. You will then lie flat on your back for several hours. Usually, you will be able to go home the same day, but there is a small chance you will be observed overnight and discharged in the morning. During a period of regular follow-up appointments, which can include ultrasound or other imaging tests, your Endovascular interventionist will monitor your progress after the therapy.
Deep Vein Disease
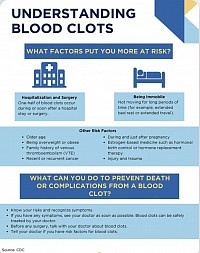
Blood clots in the veins are known as deep vein thrombosis (DVT) and can travel to the lungs, becoming a pulmonary embolism (PE). Learn more about the signs, symptoms and risk factors that contribute to blood clot development.
Are there other forms of DVD
Chronic venous insufficiency due to Varicose Veins
Chronic venous insufficiency describes the disorder of veins preventing the backflow of blood back to the heart, which commonly leads to pooling of blood in the legs.
May–Thurner syndrome
When the right iliac artery (the main blood vessel for the right leg) rests on top of the left iliac vein (the main vein draining the left leg in the pelvis), causing pressure, the result is named May–Thurner syndrome. This pressure on the left iliac vein can cause blood to flow abnormally, which can have serious consequences. May–Thurner syndrome is also known as iliac vein compression syndrome, iliocaval compression syndrome or Cockett syndrome.
Outside of Endocacular interventional, May–Thurner syndrome can be difficult to diagnose, but it should be considered as it has been shown to increase the likelihood of developing DVT in addition to other symptoms, such as pelvic pain, that can result from pelvic vein dilation.
How do End Vas Int treat deep venous disease?
Blood-thinning medication:
The main treatment for VTE is blood-thinning medication. Blood thinners are given to stop new clots from forming. In patients who cannot receive blood thinners, have additional clot formation despite blood-thinning medication or have a particularly large amount of clotting, an interventionist may place a filtering device in the affected vessel or perform an interventional treatment described below.
Interventional treatment of deep vein thrombosis: With each treatment, an interventionist makes a small incision to access the femoral vein (the large vein in the thigh). Guided by flouroscope, the doctor inserts a catheter (a thin plastic tube) through the vein to the DVT (clot) site.
Thrombolysis
Using imaging guidance, Interventionist place specialized catheters within a blood clot. These catheters will allow clot-melting medication, called tissue plasminogen activator (TPA), to be injected directly into the clot. This allows for complete treatment of the blood clot over 1–2 days. During this treatment, people are often placed in the intensive care unit (ICU) for closer monitoring. In some cases, this can be offered in combination with mechanical thrombectomy, a procedure to remove the clot.
Mechanical thrombectomy
With mechanical thrombectomy, the interventionist guides a device through the veins to the DVT site. Once there, the doctor uses the devices that are available to remove the clot. Occasionally, the clot needs to be broken up into smaller pieces to allow for removal.
Angioplasty and stenting
After treating the blood clot, the interventionist may find a stenosis, which is a narrowing in the vein that limits blood flow. The stenosis can be treated by angioplasty, where inflating a balloon makes the vein larger. In some situations, a metal tube called a stent may need to be placed as a scaffold to widen the vein, propping the vein open to allow blood flow and prevent the vein from narrowing again.
Inferior vena cava filter (IVC filter)
For people who cannot tolerate other treatments, a filtering device may be placed within the inferior vena cava (IVC), the large vein in the abdomen that drains the blood from the legs. The IVC filter acts like a small net, allowing for normal blood flow, but catching any traveling blood clots, preventing a DVT from moving to the lungs. Additionally, most IVC filters will be removed once the blood clot has cleared or when you can begin taking blood thinners to treat the clot.
What is the treatment’s recovery like?
Because many of these treatments are performed in emergency situations, you may have to stay in the hospital for observation to ensure additional clots do not form or travel to the lung causing pulmonary embolism. However, due to the minimally invasive nature of the treatments performed by an interventionist, the recovery time for the procedure is normally very short. Once you are released from the hospital, you can resume normal activity if cleared by your doctor.
Your interventionist will likely prescribe blood thinners to prevent more clots from forming after treatment. Additionally, you may be advised to wear compression stockings to help manage leg swelling.
During your follow-up appointments, your interventionist will evaluate your progress and address any remaining issues or symptoms that you may have. If your treatment included an IVC filter, your Interventionist will develop a care plan to ensure that the filter is removed at the appropriate time once the clots have cleared.
What are the risks of the treatments?
For patients who received blood thinners, there is a risk of excessive bleeding or clotting if your blood is not kept at the correct consistency. Your physician will monitor the thickness of your blood to ensure that it is within an appropriate range for you to avoid these side effects.
For patients who received IVC filters, there is a small risk that the filter can travel if it is left in place for too long. This is why it is part of the care plan to retrieve the filter after the clot has dissolved and the filter is no longer needed.
As with any treatment that involves puncture to the skin, there is a small risk of infection at the site of treatment.